Let’s talk about sexual health – a complex and multifaceted aspect of overall wellness, influenced by personal, psychological, relational, cultural, spiritual, physical, and emotional factors. To define it, it is as individual and complicated as the various dynamics of our lives, encompassing the ability to have pleasurable and safe sexual experiences, free of coercion, discrimination, and violence, and involves a positive and respectful approach to sexual relationships.
Recognizing the diversity of human sexuality is crucial, as it underscores the importance of sexual health as a fundamental aspect of overall health and well-being.
Sexual health is interconnected with both emotional health and mental health, highlighting the importance of a holistic approach to well-being.
As a physical therapist, I’ve seen firsthand patients struggling with sexual dysfunction– whether it’s pain during intercourse, difficulty achieving orgasm, or urinary incontinence during sex.
Many of these patients are surprised to learn that the root cause of their problems may be their pelvic floor muscles. But the good news is that with the right care and exercises, you can improve the health of your pelvic floor muscles and enhance your sexual well-being. So let’s explore the connection between sexual health and pelvic floor muscles!
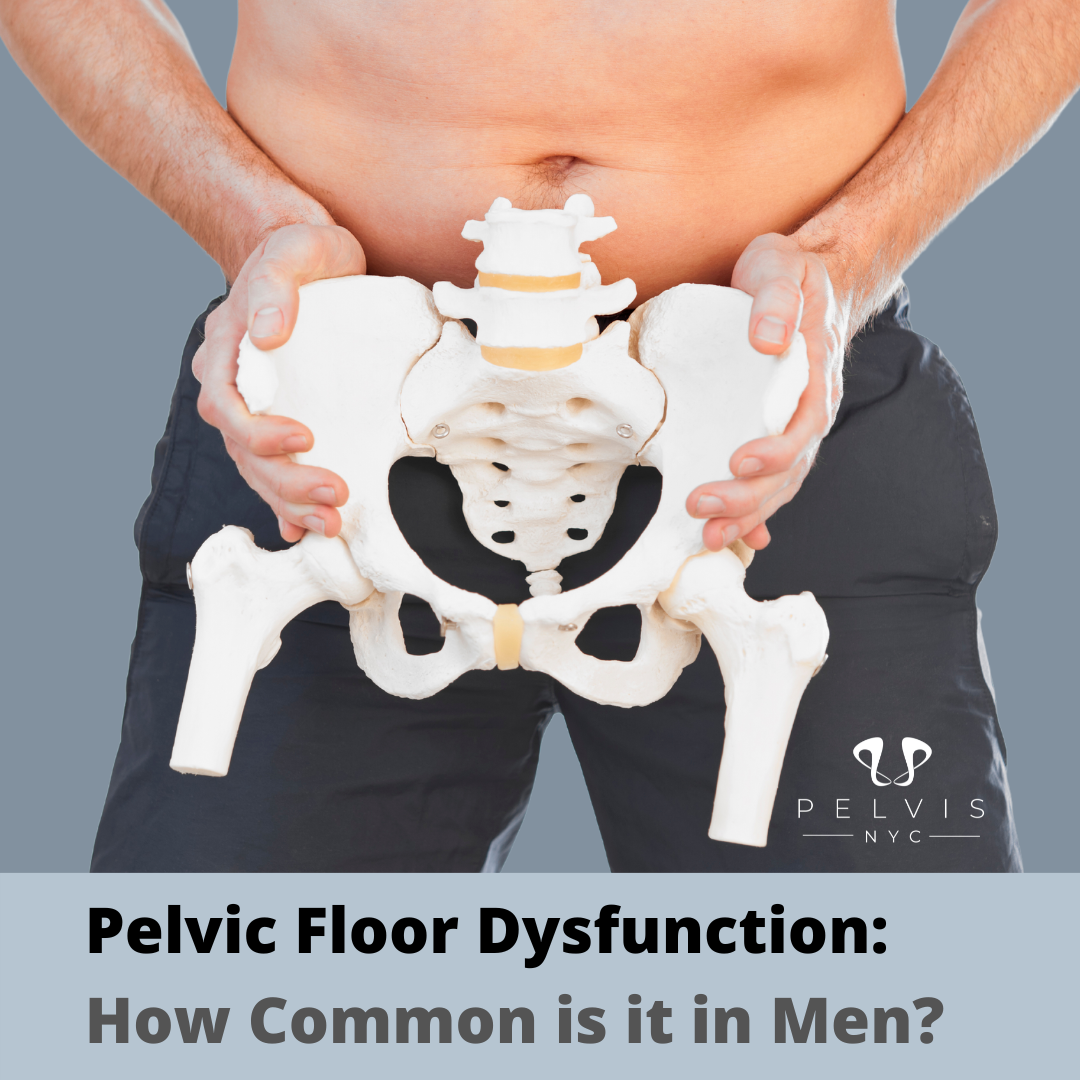
Anatomy of the Pelvic Floor Muscles and Reproductive Health
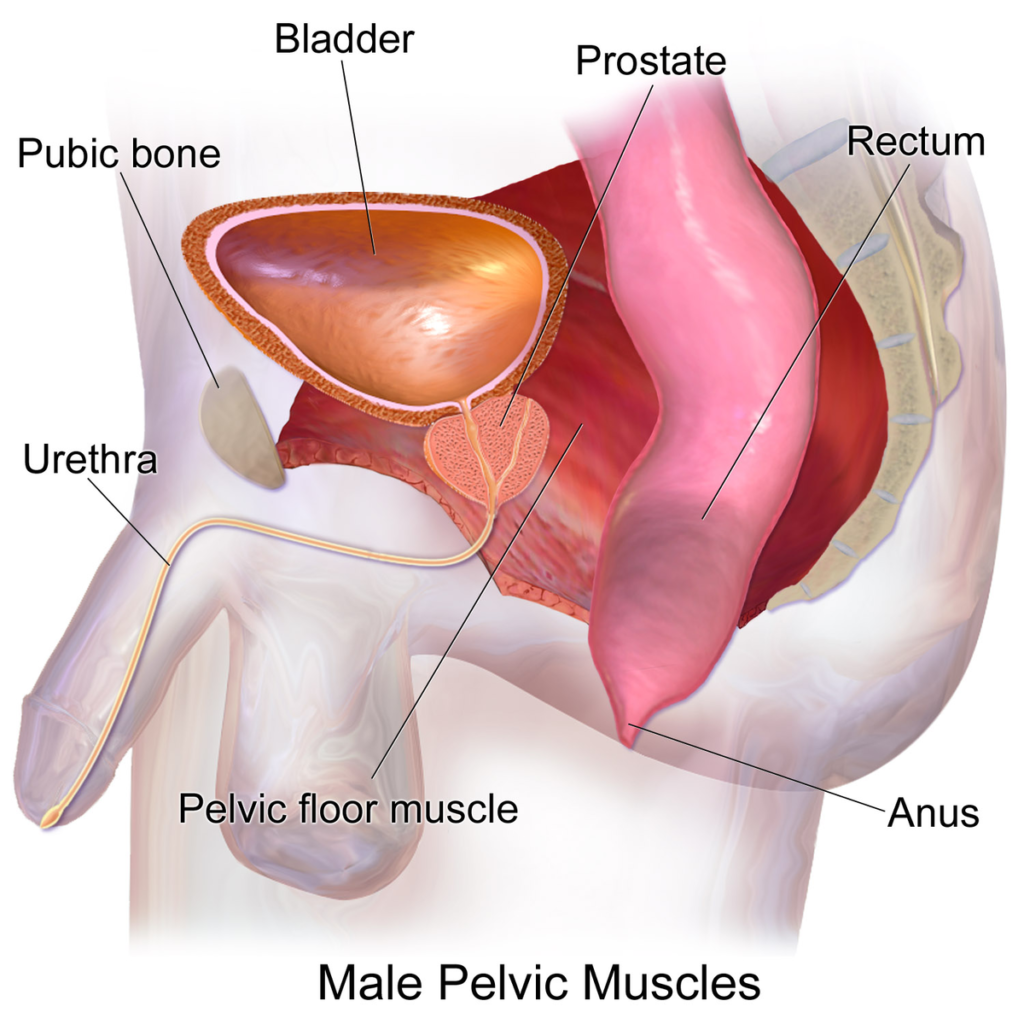
To understand why pelvic floor muscles are important for sexual health, it’s essential to know their anatomy. A pelvic floor is a group of muscles that stretch from the pubic bone at the front of the pelvis to the tailbone at the back. These muscles form a sling that supports the bladder, rectum, and other pelvic organs.
Sexual orientation can influence sexual health, making it important to understand and respect different orientations. This includes recognizing how someone is attracted sexually, emotionally, and romantically, and acknowledging that sexual orientation can be fluid and change over time.
How Pelvic Floor Muscles Affect Sexual Health and Sexual Relationships

So why do pelvic floor muscles matter for sexual health? The answer lies in their role in sexual function. The pelvic floor muscles play a crucial role in achieving and maintaining an erection in men. Strong pelvic floor muscles can also help with achieving orgasm and maintaining control over ejaculation during sexual activity.
But when pelvic floor muscles are weak or tight, they can interfere with sexual function. Men may experience erectile dysfunction or premature ejaculation, while women may have difficulty achieving orgasm or experience pain during intercourse. Also, pelvic floor muscle dysfunction can lead to urinary or fecal incontinence during sex, which can cause sharp pain during sexual intercourse.
Healthy sexual relationships and sexual expression are essential components of overall sexual health. Promoting a positive and respectful approach to sexuality can enhance pleasurable and safe sexual experiences.
Pelvic Floor Exercises for Sexual Health Information:
Pelvic floor muscle exercises, also known as Kegels, are a simple and effective way to improve pelvic floor strength and optimize sexual function. These exercises involve contracting and relaxing the pelvic floor muscles, similar to stopping and starting urine flow. To perform Kegels, sit comfortably and squeeze your pelvic floor muscles for a few seconds. Relax for the same amount of time. Repeat this exercise 10-15 times, 3 times per day.
Physical Therapy for Pelvic Floor Dysfunction: Benefits for Physical and Mental Health
If you are experiencing sexual dysfunction or other symptoms related to pelvic floor muscles, seeking the help of a physical therapist is a wise choice. A physical therapist can evaluate your pelvic floor muscles, develop an individualized treatment plan, and teach you exercises to improve strength and coordination. Treatment may also include manual therapy, biofeedback, and relaxation techniques to help reduce muscle tension and improve sexual function, contributing to better physical and mental health.
Reproductive health is also crucial when addressing pelvic floor dysfunction, as it encompasses access to necessary medical care and services.
In addition to physical therapy, fostering healthy relationships is essential for overall well-being and sexual health.
Conclusion:
Your pelvic floor muscles are an essential component of your overall health, including sexual health. Providing empowering sexual health information can help individuals understand the importance of maintaining strong pelvic floor muscles. By performing pelvic floor exercises and seeking the guidance of a physical therapist, you can improve your pelvic floor function and enhance your sexual experience. Don’t hesitate to seek help if you are experiencing symptoms related to pelvic floor dysfunction. Visit www.pelvis.nyc now!
Remember, a healthy pelvic floor leads to a healthy sex life. It is crucial to adopt a positive and respectful approach to sexual health.