Have you ever felt like something just isn’t quite right in your pelvic area — maybe a sense of tightness, discomfort, or even unexplained pain? You’re not alone, and the good news is that there’s a path to relief. As a physical therapist specializing in pelvic health, I’m passionate about helping people understand their bodies and feel empowered on their journey toward healing. One condition I often see in my practice is called hypertonic pelvic floor dysfunction. It is characterized by excessively tense pelvic floor muscles that cannot relax, and understanding it is the first step toward finding lasting comfort.
What Is Hypertonic Pelvic Floor?
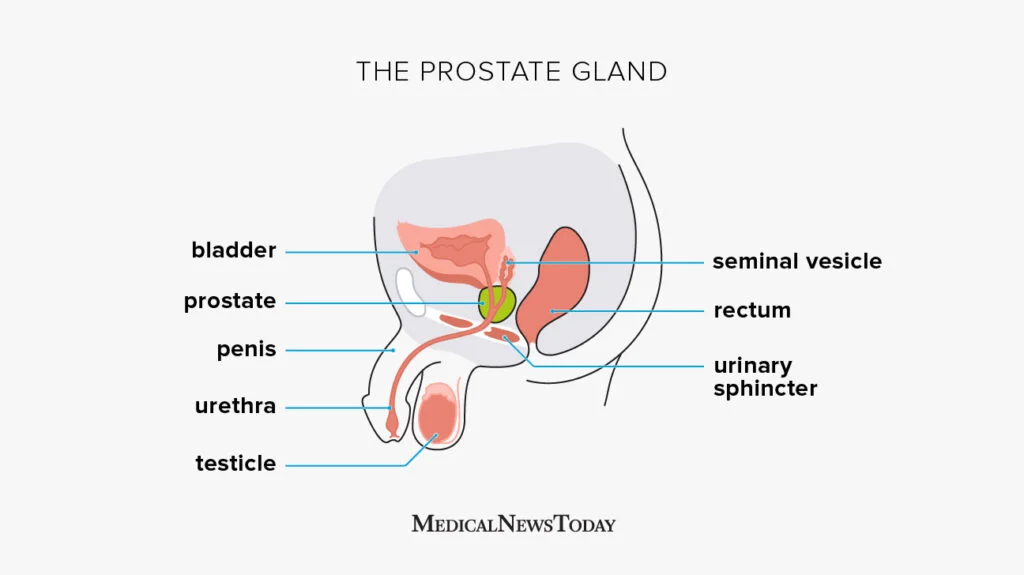
In simple terms, hypertonic pelvic floor means the muscles in your pelvic region are too tight. Think of these muscles as a hammock that supports your bladder, uterus (if you have one), rectum, and other pelvic organs. Normally, these muscles should contract and relax as needed. But when they become hypertonic, they remain in a constant state of contraction, creating tension and discomfort. This condition, known as hypertonic pelvic floor muscles, can affect individuals across different genders and may be mistaken for other conditions, leading to frequent misdiagnosis despite its commonality.
Hypertonic Pelvic Floor Dysfunction
It’s important to understand that hypertonic pelvic floor is actually a type of pelvic floor dysfunction (PFD), but not all PFD is due to hypertonicity. Pelvic floor dysfunction is a broad term used to describe any condition where the pelvic floor muscles aren’t functioning properly. This can include muscles that are too tight (hypertonic), too weak (hypotonic), or uncoordinated. Identifying the specific type of dysfunction is key to finding the right treatment. It can be challenging to diagnose pelvic floor dysfunction, as symptoms often manifest in various parts of the body, complicating accurate diagnosis.
Understanding Hypertonic Pelvic Muscles
Just like any other muscle in your body, your pelvic floor muscles can become overactive or tense. Imagine clenching your jaw all day — eventually, you’d start feeling pain, fatigue, and perhaps even issues with eating or talking. The same principle applies to your pelvic floor. Hypertonic pelvic muscles don’t get the rest they need, and over time, this can lead to a host of symptoms that affect your daily life, including chronic pelvic pain.
What Does a Hypertonic Pelvic Floor Feel Like?
Experiencing a hypertonic pelvic floor can be quite varied and often distressing. Many people describe a persistent feeling of tightness or tension in the pelvic area, which can come and go or be a constant presence. This tightness can lead to pain or discomfort in the pelvic floor, vagina, bladder, or anus, with the intensity ranging from mild to severe.
You might find it difficult to start or stop the flow of urine, or you may feel like your bladder never fully empties. Similarly, bowel movements can become a struggle, with straining or discomfort and a sensation that your bowels are not completely empty.
Sexual activity can also be affected, with pain or discomfort during intercourse, which can be felt in the vagina, penis, or anus. Some people report a feeling of pressure or heaviness in the pelvic area, which can worsen with certain activities or positions. Additionally, muscle spasms or cramping in the pelvic floor can occur, which can be intense and debilitating.
These sensations can significantly impact daily life, making it crucial to seek medical attention if you experience persistent or worsening symptoms. Understanding these feelings is the first step towards finding relief and improving your quality of life.
Diagnosing Pelvic Floor Dysfunction and Nonrelaxing Pelvic Floor
Diagnosing pelvic floor dysfunction, especially when hypertonicity is involved, requires a specialized assessment. A physical therapist or healthcare provider will conduct a thorough evaluation that may include:
- Patient History: Understanding symptoms, lifestyle, and any contributing factors.
- Physical Examination: This may involve external assessment of posture, breathing, and movement patterns, as well as internal examination to assess muscle tone, tenderness, and coordination.
- Biofeedback Testing: Using sensors can measure muscle activity and provide insight into how well the pelvic floor muscles relax and contract.
Chronic pain is often a significant symptom of nonrelaxing pelvic floor muscle dysfunction. This can impact the quality of life and necessitate proper identification and management.
Nonrelaxing pelvic floor is a condition closely related to hypertonicity. It happens when the pelvic floor muscles are unable to fully relax, even when they should. This constant tension can lead to chronic discomfort and dysfunction, making proper diagnosis essential for effective treatment.
Hypertonic Pelvic Floor Symptoms
Recognizing the hypertonic pelvic floor symptoms is the first step toward healing. Here are some common symptoms:
- Pelvic Pain: This can present as a constant ache, sharp pain, or a feeling of heaviness in the pelvic area.
- Painful Intercourse: Many people with hypertonicity pelvic floor experience discomfort or pain during sex, known as dyspareunia.
- Urinary Issues: Frequent urination, difficulty starting the flow, or a sensation of incomplete emptying are common.
- Constipation or Straining: Tight pelvic muscles can make it hard for stool to pass, leading to constipation.
- Low Back, Hip, or Groin Pain: The pelvic floor muscles connect to other structures in the body, so tightness can radiate to nearby areas.
- Difficulty Relaxing: Many people report a constant feeling of tension or an inability to “let go” in the pelvic region.
- Irritable Bowel Syndrome: This condition is associated with chronic pelvic pain and can be linked to the interconnectedness of the pelvic organs.
Why Do Pelvic Floor Muscles Become Hypertonic?
There are several reasons why hypertonic pelvic floor occurs:
- Chronic Stress: Stress can cause muscles to tighten, including those in the pelvic floor.
- Injury or Trauma: Physical injuries, surgeries, or even emotional trauma can lead to muscle guarding and hypertonicity.
- Posture and Movement Patterns: Poor posture or habits like clenching your glutes can contribute to pelvic floor tension.
- Overuse: Activities that require constant engagement of the pelvic muscles, like heavy lifting or high-impact sports, can lead to tightness over time.
Can Hypertonicity Pelvic Floor Be Cured?
Yes, hypertonicity pelvic floor can be effectively treated, and many people experience significant relief with the right approach. Recovery often involves a combination of physical therapy, lifestyle changes, and consistent self-care to address pelvic floor muscle tension. The key is identifying the root cause and addressing it with a personalized treatment plan tailored to your body’s needs.
Why Physical Therapy Is Essential in Treating Hypertonicity Pelvic Floor
Physical therapy is fundamental in treating hypertonicity pelvic floor because it addresses both the symptoms and the root cause of the condition. A skilled pelvic health physical therapist can assess your unique muscle patterns and develop a personalized plan to restore balance. Through hands-on techniques, guided exercises, and education, physical therapy empowers you with the tools and knowledge to relax your pelvic floor, relieve pain, and prevent future issues. Additionally, physical therapy can be highly effective in managing various pelvic floor disorders, ensuring comprehensive care for a range of symptoms.
Treatment Options for Hypertonicity Pelvic Floor
The good news is that the hypertonicity pelvic floor is treatable! As a physical therapist, I often guide my patients through personalized treatment plans that may include:
- Manual Therapy: Hands-on techniques to gently release tension in the pelvic muscles.
- Breathing Exercises: Diaphragmatic breathing helps activate the parasympathetic nervous system, promoting muscle relaxation.
- Pelvic Floor Down-Training: Techniques to teach the muscles how to relax and lengthen, rather than staying in a constant state of contraction.
- Stretches and Gentle Movement: Specific stretches targeting the hips, lower back, and inner thighs can help alleviate tightness.
- Biofeedback: This technique involves using sensors to monitor muscle activity, helping you gain better control over pelvic floor relaxation.
- Behavioral Modifications: Addressing habits like breath-holding, glute clenching, or poor posture can make a big difference over time.
- Bowel Movement Management: Techniques to ease difficulty in passing bowel movements by promoting relaxation of the pelvic floor muscles.
Tips for Preventing Hypertonicity Pelvic Floor
Prevention is key when it comes to pelvic health. Here are some tips to help keep your pelvic floor muscles balanced and healthy:
- Manage Stress: Practice mindfulness, meditation, or other stress-reduction techniques. This helps prevent chronic muscle tension, which can contribute to hypertonic pelvic floor muscles.
- Breathe Properly: Focus on deep, diaphragmatic breathing to naturally relax your pelvic floor.
- Maintain Good Posture: Avoid slouching and ensure your pelvis is in a neutral position when sitting or standing.
- Avoid Over-Clenching: Be mindful of habits like constantly squeezing your glutes or holding tension in your abdomen.
- Stay Active: Gentle movements like walking, yoga, or swimming can promote pelvic floor health without overloading the muscles.
- Listen to Your Body: If you start feeling tension or discomfort, take a moment to stretch and relax.
How Pelvis NYC Can Help
At Pelvis NYC, we understand that everybody is unique, and so is every healing journey. Our team of pelvic health physical therapists dedicates themselves to helping you find relief from hypertonic pelvic floor dysfunction symptoms and empowering you with the tools to prevent future issues. We offer personalized treatment plans, hands-on therapy, and education to help you reconnect with your body and regain control over your pelvic health.
If any of these symptoms resonate with you, please know that you don’t have to live with the discomfort. Seeking help from a pelvic health specialist can make a world of difference. Your body deserves care and attention, and taking that first step toward healing is a brave and powerful decision.
Let your healing journey begin — you deserve to feel good in your body again.
How Pelvis NYC Can Help
At Pelvis NYC, we understand that everybody is unique, and so is every healing journey. Our team of specialized pelvic health physical therapists is dedicated to helping you find relief from hypertonicity pelvic floor symptoms and empowering you with the tools to prevent future issues. We offer personalized treatment plans, hands-on therapy, and education to help you reconnect with your body and regain control over your pelvic health.
If any of these symptoms resonate with you, please know that you don’t have to live with the discomfort. Seeking help from a pelvic health specialist can make a world of difference. Your body deserves care and attention, and taking that first step toward healing is a brave and powerful decision.
Let your healing journey begin — you deserve to feel good in your body again. Book an appointment with Pelvis NYC today and take the first step toward a pain-free life.