Enlarged prostate, also known as Benign Prostatic Hyperplasia (BPH) or Benign Prostatic Enlargement (BPE), is typically seen as a condition affecting older men, often those over 50. However, it’s important to recognize that younger males can also experience BPH, although it is much less common. In this post, we’ll explore the factors contributing to BPH in younger men, the symptoms to watch for, and how they can be managed effectively.
What Is Benign Prostatic Hyperplasia and How Does It Develop?
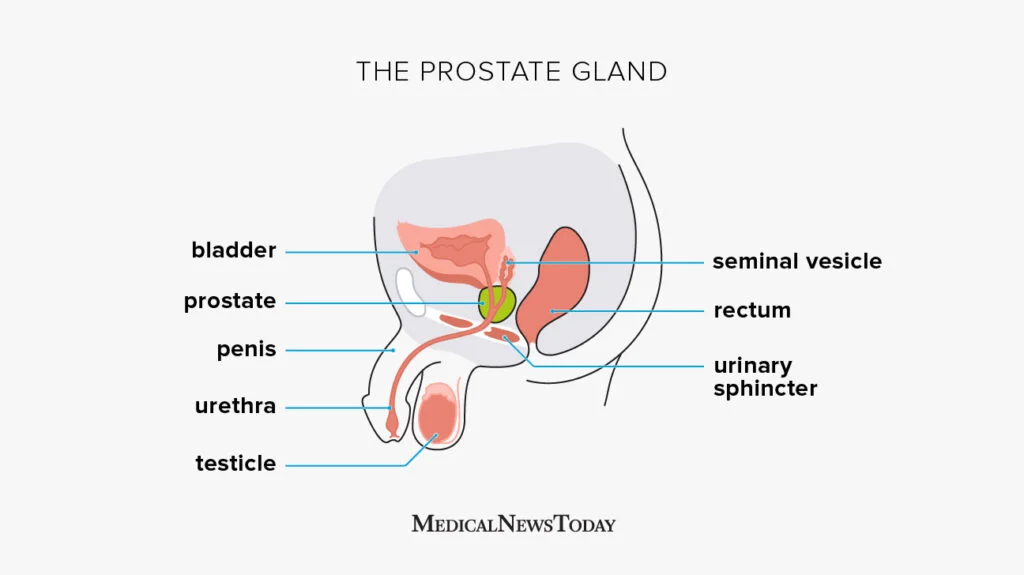
BPH occurs when the cells of the prostate gland begin to multiply, leading to an increase in the size of the prostate. This enlargement can compress the urethra and cause urinary difficulties. Lower urinary tract symptoms, such as issues with urinary flow and frequency, are common indicators of prostate health problems.
While BPH is most often linked to aging, the underlying causes are multifaceted and include hormonal changes, genetics, and lifestyle factors. BPH symptoms can vary, including obstructive symptoms like urinary incontinence and burning during urination, complicating the understanding and diagnosis of the condition. As men age, their testosterone levels decrease while levels of dihydrotestosterone (DHT), a hormone that stimulates prostate growth, increase. These shifts in hormones are believed to be a significant trigger for prostate enlargement.
Causes and Risk Factors of BPH in Younger Males
Benign prostatic hyperplasia (BPH) is a complex condition, and its exact causes are not fully understood. However, several factors are thought to contribute to the development of BPH. These include:
- Hormonal Changes: As men age, the balance of sex hormones in their bodies changes. This can lead to an increase in the production of dihydrotestosterone (DHT), a hormone that promotes the growth of prostate tissue.
- Genetics: Men with a family history of BPH are more likely to develop the condition.
- Age: BPH is more common in men over 50.
- Obesity: Being overweight or obese may increase the risk of developing BPH.
- High Blood Pressure: Men with high blood pressure are more likely to develop BPH.
- Diabetes: Men with diabetes are more likely to develop BPH.
- Lack of Exercise: A sedentary lifestyle may increase the risk of developing BPH.
Understanding these risk factors can help take proactive steps to manage and potentially reduce the risk of developing benign prostatic hyperplasia BPH.
Can BPH Affect Younger Males?
Though rare, younger males can develop BPH, typically under the age of 40. When this happens, it’s often due to several contributing factors:
- Genetics: Family history plays a big role. If close relatives have experienced BPH, younger men may be more predisposed to developing it.
- Lifestyle Choices: Diets high in fat, lack of physical activity, and excessive alcohol consumption have been linked to an increased risk of early prostate enlargement.
- Hormonal Imbalances: Medical conditions or medications that affect hormone levels can lead to the acceleration of prostate growth. Erectile dysfunction can also be a concern, as treatments for BPH, such as phosphodiesterase-5 inhibitors like Cialis, may address both conditions.
- Other Health Conditions: Conditions like prostatitis (inflammation of the prostate) can mimic the symptoms of BPH and affect younger men as well. Additionally, any urinary tract infection should be effectively treated before considering surgical options, as it could complicate outcomes and recovery.
Lower Urinary Tract Symptoms of BPH in Younger Men
The symptoms of BPH are generally similar regardless of age. However, younger men may notice some distinct differences. Common signs to watch for include:
- Frequent Urination: This is especially problematic at night (nocturia), which can disrupt sleep and daily activities.
- Difficulty Starting Urination: A hesitancy or delay in initiating urination can be a frustrating experience.
- Weak Urine Stream: A slow or intermittent stream may lead to the sensation of not fully emptying the bladder.
These symptoms can be related to the bladder neck, where the urethra joins the bladder, located just below the prostate.
If you’re a younger man experiencing any of these symptoms, it’s important to consult a healthcare provider for an accurate diagnosis.
Diagnosing BPH in the Prostate Gland of Younger Men
If you’re experiencing urinary symptoms, your doctor will likely perform a series of tests to determine the cause. These may include:
- Physical Exam & Medical History: Your doctor will discuss your symptoms, lifestyle, and any family history of prostate issues.
- Blood Tests: Bloodwork can assess kidney function, hormone levels, and prostate-specific antigen (PSA) levels, which may indicate prostate problems.
- Imaging Tests: Ultrasound or other imaging techniques can help assess the size and shape of the prostate.
- Urine Flow Test: This test measures the strength and flow of your urine to check for any blockages or obstructions.
For men who have not responded to medical therapies or who have experienced complications, surgical treatment can help prevent long-term deterioration of bladder function.
Complications and Related Conditions
If left untreated, BPH can lead to several complications, including:
- Urinary Retention: The inability to urinate, which can lead to kidney damage and other serious health problems.
- Kidney Damage: The bladder can become overworked, leading to kidney damage and other complications.
- Bladder Damage: The bladder can become stretched and weakened, leading to incontinence and other problems.
- Incontinence: The loss of bladder control, which can lead to embarrassing and inconvenient situations.
- Recurrent Urinary Tract Infections: BPH can increase the risk of developing urinary tract infections, which can be painful and uncomfortable.
- Prostate Cancer: While BPH is not a direct cause of prostate cancer, it can increase the risk of developing the disease.
Recognizing these potential complications underscores the importance of early diagnosis and effective management of BPH to maintain overall health and quality of life.
Managing BPH in Young Males
If BPH is diagnosed, there are several ways to manage the condition and prevent it from worsening. These treatments may include:
- Pelvic Floor Therapy: As a physical therapist, I often recommend pelvic floor exercises to help improve bladder control and alleviate symptoms. These exercises strengthen the muscles around the prostate and bladder, improving their coordination.
- Lifestyle Changes: Diet, exercise, and reducing alcohol consumption can all help maintain prostate health. A healthy lifestyle may also slow the progression of BPH.
- Medications: Alpha-blockers and other medications may be prescribed to relax the muscles around the prostate, easing symptoms like slow urination. Minimally invasive procedures are also available as recent alternatives to surgery for managing symptoms and improving urinary flow.
- Regular Checkups: Regular follow-ups with your healthcare provider allow for monitoring of symptoms and early intervention when necessary. Alpha-adrenergic blockers, originally designed for high blood pressure, can relax prostate muscle tissue and subsequently relieve urinary frequency and nocturia symptoms associated with BPH.
Proactive Steps for Your Prostate Health
It’s crucial to pay attention to prostate health, regardless of your age. If you’re noticing symptoms, here are a few questions to consider:
- Could making lifestyle changes help reduce my symptoms?
- Is pelvic floor therapy something I should try for better prostate management?
- Should I consult a urologist to get a full diagnosis?
At Pelvis NYC, we specialize in men’s health and pelvic floor therapy. If you’re ready to take proactive steps toward managing BPH or prostate health, our team is here to guide you. Visit us at www.pelvis.nyc for more information and support.
When to See a Doctor
If you are experiencing any of the following symptoms, it is essential to see a doctor:
- Difficulty starting to urinate
- Weak or interrupted urine flow
- Frequent urination, especially at night
- Feeling like the bladder is not fully empty
- Painful urination
- Blood in the urine
- Painful ejaculation
- Pain in the lower back or pelvis
Early diagnosis and treatment can help alleviate symptoms and prevent complications. If you are experiencing any of these symptoms, do not hesitate to seek medical attention. Taking prompt action can significantly improve your quality of life and prevent more serious health issues down the line.